Some medical residents, or doctors in training, at UW Hospital who are exposed to COVID-19 patients said they haven’t been able to get vaccinated, even as some staff doctors with less exposure have received shots.
Providers such as physician assistants and nurse practitioners who haven’t been immunized have refused to see infected patients, while unvaccinated residents can’t refuse, the residents said.
“We are asked to bear an outsized amount of the risk while being afforded less protection than other people,” said a surgical resident who asked to remain anonymous for fear of workplace retaliation. “To us as residents this is a part of a pattern in which we are consistently deprioritized in terms of our safety.”
UW Health spokesman Tom Russell said “it’s not our practice” for staff doctors to get shots before residents with more exposure or to let other providers refuse care if unvaccinated.
Spokesman Andrew Hellpap said in a statement that the organization “has vaccinated thousands of faculty and staff involved in direct patient care, including several hundred residents and fellows.”
He said the system plans to start immunizing more residents soon. “Given we have built capacity to administer about 600 vaccine doses per day, our limiting factor in how quickly we can move through our population is the supply of COVID-19 vaccine,” Hellpap said.
Priority is given based on “estimated frequency, duration and intensity of exposure” to patients with known or suspected COVID-19 and guided by “an equity framework that examines risk of exposure, along with age” and social vulnerability, he said.
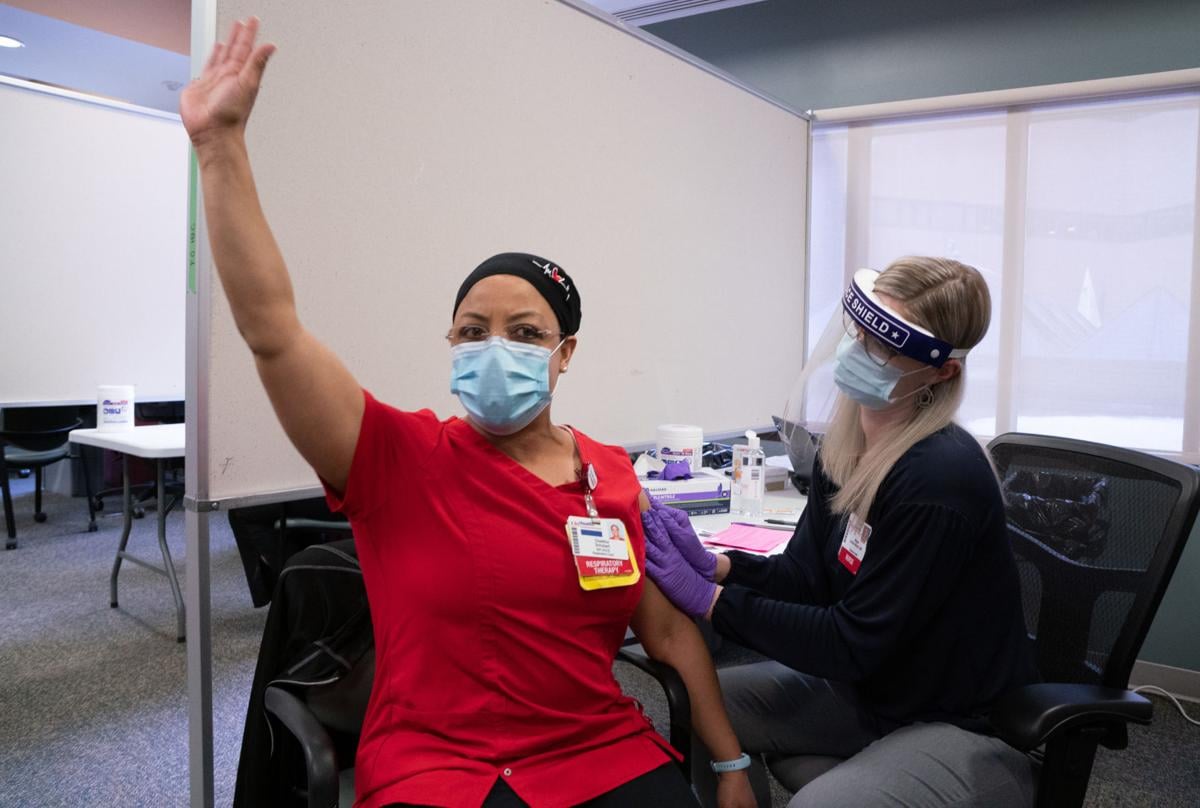
UW Health last week got 3,900 doses of Pfizer’s COVID-19 vaccine and said it was first inoculating doctors, nurses, respiratory therapists and others in intensive care, emergency medicine and other settings that make them most exposed to COVID-19 patients. Hellpap declined to say if UW Health got more vaccine this week or when it will, but nationally most if not all health care workers are expected to be offered immunization by next month.
Federal officials have designated health care workers and nursing home residents as the top priority groups.
Three UW Hospital surgical residents — doctors who care for patients during additional training required after medical school — interviewed by a Wisconsin State Journal reporter said they represented concerns of dozens of colleagues. Each requested anonymity, citing concerns about retaliation.
The residents said staff doctors have been vaccinated before residents, who spend more time in the emergency room or intensive care treating infected or potentially infected patients and sometimes perform high-risk procedures.
Physician assistants and nurse practitioners who haven’t been vaccinated can opt out of seeing COVID-19 patients, which the residents said was fine, but they can’t.
On a hospital unit with a COVID-19 outbreak, many staff including nurses were vaccinated but residents were not, the residents said.
The residents said they were told they weren’t given higher priority because of a clerical error in which their time in the emergency room wasn’t taken into account, but that an administrator said the error couldn’t be fixed.
Residents in internal medicine, family medicine and critical care have rightly been immunized before surgical residents, but the surgical residents should get priority before staff doctors who have less exposure to COVID-19 patients, the residents said.
“Enough is enough,” one of the residents said.
“We all feel like we’re put at the bottom,” another said.
Residents in some parts of the country have moved to form unions to counter what they see as a decades-old culture of working overtime for relatively little pay. In 2003, the national organization that oversees residency programs said residents could work no more than 80 hours a week.

COMMENTS